Kenneth A. Eilertsen, Morten Winberg, Elisabeth Jeppesen, Gyri Hval, and Torben Wisborg published the article “Prehospital Tourniquets in Civilians: A Systematic Review” in the Prehospital and Disaster Medicine in 2021.
The authors conducted an examination of tourniquet use in civilian environments across 55 studies. These studies reported survival rates ranging from 87% to 100%. It’s crucial to note that none of the studies were randomized controlled trials, and those with comparison groups faced challenges due to unclear indications for tourniquet placement and potential bias stemming from more severe injuries in the tourniquet group.
Regarding military studies, they reported similar mortality rates for patients treated with tourniquets and those without, even though the tourniquet group had more severe injuries. Early tourniquet application before the onset of shock was strongly associated with increased survival. For example, one study revealed a 96% survival rate when tourniquets were applied before shock onset compared to only 4% for those receiving tourniquets later.
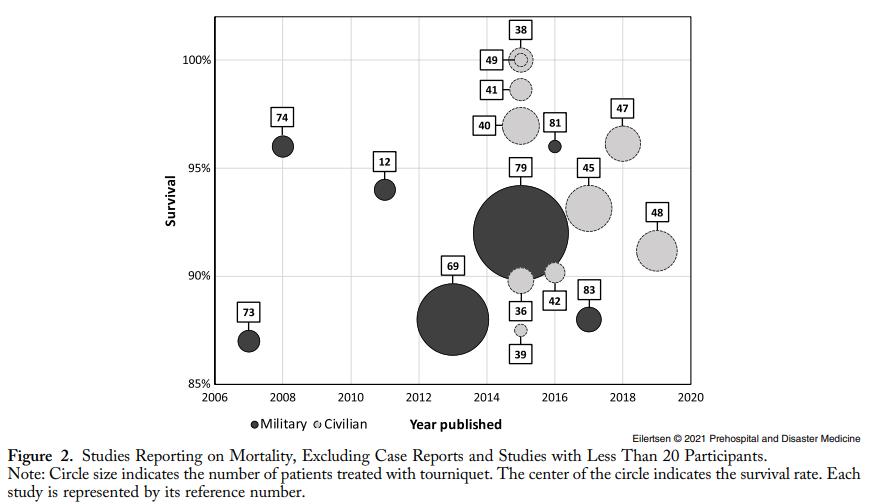
In the civilian setting, studies suggested a survival benefit for patients treated with tourniquets. Those who received prehospital tourniquets had a lower incidence of shock upon hospital arrival compared to those without tourniquet treatment. Additionally, one study highlighted that death from hemorrhagic shock was more frequent among patients who received in-hospital tourniquets (14%) than among those who received prehospital tourniquets (3%). Most studies also reported an average tourniquet application time of less than two hours.
Complications associated with tourniquet use were reported in thirty-five studies, with 21 in civilian and 14 in military settings, including ten case reports. Notably, fifteen studies mentioned nerve palsy linked to tourniquets. In civilian studies, nerve palsies affected 18 of 465 patients in six studies. One study found no tourniquet-related nerve palsies. Amputations linked solely to tourniquets were very rare, mainly associated with improvised tourniquets and prolonged application times.
Fasciotomy and compartment syndrome were reported in 17 studies, including three case reports. Fasciotomy was a common treatment following tourniquet use, and compartment syndrome was more likely without fasciotomy, especially with tourniquet application times exceeding two hours.
Seven studies addressed infections linked to tourniquet use, with five civilian and two military studies. Among 764 tourniquet-treated civilian patients, 67 experienced wound infections (nine percent). Tourniquet use did not significantly impact secondary infection rates when compared to non-tourniquet groups.
“Despite low level of evidence in the studiesidentified, the studies consistently indicated that the use of a tourniquet was associated with increased survival in uncontrollable extremity bleeding in a civilian setting. The civilian and military studies reported similar findings and treatment efficiency, though military studies tended to have longer application times. Complications to tourniquet use seemed to be tightly related to application time, and application times less than two hours seemed to be reasonably safe in previously healthy patients. Application times in urban civilian settings were short.”
Eilertsen, K., Winberg, M., Jeppesen, E., Hval, G., & Wisborg, T. (2021)
Eilertsen, K., Winberg, M., Jeppesen, E., Hval, G., & Wisborg, T. (2021). Prehospital Tourniquets in Civilians: A Systematic Review. Prehospital and Disaster Medicine, 36(1), 86-94. doi:10.1017/S1049023X20001284